Co-treatment Effect of Syzygium cumini (L.) Skeels on Indomethacin Induced Gastric Ulcer on Mice Model
DOI:
https://doi.org/10.48048/wjst.2019.6224Keywords:
Co-treatment, Syzygium cumini (L.) Skeels, indomethacin, gastric ulcer and mice modelAbstract
Syzygium cumini (L.) Skeels or SCC originally from India and Southeast Asia, commonly used as a medicinal and acted as antioxidant and anti-inflammatory plant. Indomethacin, which is a part of nonsteroidal anti-inflammatory drugs (NSAIDs) family, induced gastric damage and perforation through the excess generation of reactive oxygen species (ROS). This research focus on co-treatment administered between SCC and indomethacin in the subsequent 7 days and evaluated on oxidative damage, inflammatory parameter and epidermal growth factor (EGF) receptor. SCC showed a concentration and dose dependent reduction in ulcer index (UI) values leading to the increasing of inhibition percent when compared to indomethacin treated mice, confirmed by photographer which showed maximum efficacy on day 5 of treatment. On day 1 and day 3 of ulceration, malondialdehyde (MDA), oxidized glutathione (GSSG), nitrile contents and tumor necrosis factor-alpha (TNF-α) were increased. Gastric wall mucus and glutathione peroxidase (GPx) were down. After that gastric mucosa were recovered by healing processed and were regenerated the mucosal cap to promote EGF receptor. SCC was increased the up-regulation of COX-1 enzyme resulting in down-regulation to COX-2 expression at day 3 of ulceration. At day 5 and 7, the gastric ulceration were regenerated themselves. These all results indicated that SCC have a great protective effect against indomethacin induced gastric ulcer in in-vivo co-treatment model.Downloads
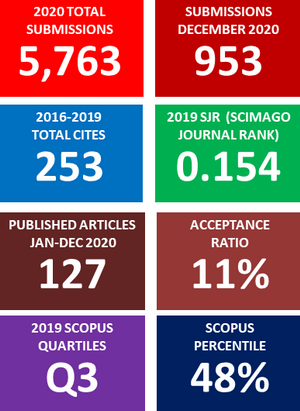
Metrics
References
M Tarique, HH Siddiqui, M Khushtar and MA Rahman. Protective effect of hydro-alcoholic extract of Ruta graveolens Linn. Leaves on indomethacin and pylorus ligation-induced gastric ulcer in rats. J. Ayurveda Integr. Med. 2016; 7, 38-43.
K Ramakrishnan and RC Salinas. Peptic ulcer disease. Am. Fam. Phys. 2007; 76, 1005-12.
T Ihamäki, K Varis and M Siurala. Morphological, functional and immunological state of the gastric mucosa in gastric carcinoma families. Comparison with a computer-matched family sample. Scand. J. Gastroenterol. 1979; 14, 801-12.
C Sostres, CJ Gargallo and A Lanas. Nonsteroidal anti-inflammatory drugs and upper and lower gastrointestinal mucosal damage. Arthritis Res. Ther. 2013; 2013, S3.
Z Halicia, B Polatb, E Cadircia, A Topcuc, E Karakusd, D Kosea, A Albayraka and Y Bayir. Inhibiting renin angiotensin system in rate limiting step by aliskiren as a new approach for preventing indomethacin induced gastric ulcers. Chem. Biol. Interact. 2016; 258, 266-75.
G Singh. Gastrointestine complications of prescription and over-the-counter nonsteroidal anti-inflammatory drugs: A view from the ARAMIS database. Am. J. Ther. 2000; 7, 115-21.
M Boyacioglu, C Kum, S Sekkin, HS Yalinkilinc, H Avci, ET Epikmen and U Karademir. The effects of lycopene on DNA damage and oxidative stress on indomethacin-induced gastric ulcer in rats. Clin. Nutr. 2016; 35, 428-35.
DE Furst, RW Ulrich and S Prakash. Nonsteroidal Anti-inflammatory Drugs, Disease-modifying Antirheumatic Drugs, Nonopioid Analgesics and Drugs used in Gout. In: BG Katzung, SB Masters and AJ Trevor (Eds.). Basic and Clinical Pharmacology. 12nd eds. McGraw Hill, USA, 2012.
MA Morsy and MA El-Moselhy. Mechanisms of the protective effects of curcumin against indomethacin-induced gastric ulcer in rats. Pharmacology 2013; 91, 267-74.
AA Asmari, SA Omani, MA Otaibi, AA Abdulaaly, I Elfaki and KA Yahya. Gastroprotective effect of minocycline in experimentally induced gastric ulcers in rats. Int. J. Clin. Exp. Med. 2014; 7, 586-96.
WIE Hinojosa, MA Quiroz, IR Alvarez, PE Castaneda, ML Villarreal and AC Taketa. Anti-Helicobacter pylori, gastroprotective, anti-inflammatory, and cytotoxic activities of methanolic extracts of five different populations of Hippocratea celastroides collected in Mexico. J. Ethnopharmacol. 2014; 155, 1156-63.
G Baldissera, NDM Sperotto, HT Rosa, JG Henn, VF Pere, DJ Moura, R Roehrs, ELG Denardin, PD Lago, RB Nunes and J Saffi. Effects of crude hydroalcoholic extract of Syzygium cumini (L.) Skeels leaves and continuous aerobic training in rats with diabetes induced by a high-fat diet and low doses of streptozotocin. J. Ethnopharmacol. 2016; 194, 1012-21.
L Chanudom and J Tangpong. Scavenging activities and protective effects of Syzygium cumini (L.) Skeels on H2O2 induced oxidative stress in normal human peripheral blood mononuclear cells. J. Health Res. 2015; 29, 315-22.
L Chanudom, P Bhoopong, R Khwanchuea and J Tangpong. Antioxidant and antimicrobial activities of aqueous & ethanol crude extracts of 13 Thai traditional plants. Int. J. Curr. Microbial App. Sci. 2014; 3, 549-58.
L Chanudom and J Tangpong. Anti-inflammation property of Syzygium cumini (L.) Skeels on indomethacin induced acute gastric ulceration. Gastroenterol. Res. Pract. 2015; 2015, 343642.
M Ayyanar and P Subash-Babu. Syzygium cumini (L.) Skeels: A review of its phytochemical constituents and traditional used. Asian Pac. J. Trop. Biomed. 2012; 2. 240-6.
RSB Eshwarappa, RS Iyer, SR Subbaramaiah, RS Richard and BL Dhananjaya. Antiuoxidant activity of Syzygium cumini leaf gall extracts. Bioimpacts 2014; 4. 101-7.
G Bonfanti, PR Bitencourt, KS Bona, PS Silva, LB Jantsch, AS Pigatto, A Boligon, ML Athyde, TL Gonealves and MB Moretto. Syzygium jumbos and Solanum guaraniticum show similar antioxidant properties but induced different enzymatic activities in the brain of rats. Molecules 2013; 18. 9179-94.
SJ Corne, SM Morrissey and RJ Woods. A method for the quantitative estimation of gastric barrier mucus. J. Physiol. 1974; 242, 116-17.
M Uchiyama and M Mihara. Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal. Biochem. 1978; 86, 271-8.
RM Rolland. A review of chemically-induced alterations in thyroid and vitamin A status from field studies of wildlife and fish. J. Wildlife Dis. 2000; 36, 615-35.
OH Lowry, J Nira, A Rosebrough, F Lewis and JR Rose. Folin phenol reagent protein measurement. J. Biol. Chem. 1951; 193, 265-75.
KM Miranda, MG Espey and DA Wink. A rapid, simple spectrophotometric method for simultaneous detection of nitrate and nitrite. Nitric Oxide 2001; 5, 62-71.
SK Yadav, B Adhikary, S Chand, B Maitty, SK Bandyopadhyay and S Chattopadhyay. Molecular mechanism of indomethacin-indued gastropathy. Free Radic. Biol. Med. 2012; 52, 1175-87.
D Banerjee, K Ajay, RK Bauri, SK Guha, Bandyopadhyay and C Subrata. Healing properties of malabaricone B and malabaricone C, against indomethacin-induced gastric ulceration and mechanism of action. Eur. J. Pharmacol. 2008; 578. 300-12.
O Dormond, M Bezzi, A Mariotti and AS Ruegg. Prostaglandin E2 promotes integrin αV 3-dependent endothelial cell adhesion, rac-activation, and spreading through cAMP/PKA-dependent signaling. J. Biol. Chem. 2002; 277, 45838-46.
L Laine. Stratifying the risk of clinical upper GI events in NSAID users: Results from a double-blind outcomes study. Gastroenterology 2001; 120, A552.
MHLP Souza, H Paula Lemos, RB Oliveira and FQ Cunha. Gastric damage and granulocyte infiltration induced by indomethacin in tumor necrosis factor receptor 1 (TNF-R1) or inducible nitric oxide synthase (iNOS) deficient mice. Gut 2012; 53, 791-6.
JM Mates, JM Segura, C Perez-Gomez, R Rosado, L Olalla, M Blanca and F Sanchez. Antioxidant enzymatic activities in human blood cells after an allergic reaction to pollen or house dust mite. Blood Cell Mol. Dis. 1999; 25, 103-12.
JL Wallace and MJ Miller. Nitric oxide in mucosal defense: A little goes a long way. Gastroenterology 2000; 119, 512-20.
J Piotrowski, A Slomiany and BL Slomiany. Activation of apoptotic caspase-3 and nitric oxide synthase-2 in gastric mucosal injury induced by indomethacin. Scand. J. Gastroenterol. 1999; 34. 129-34.
V Bertrand, R Guimband, M Tulliez, C Mauprivez, P Sogni, D Couturier, JP Giroud, S Chanssade and ML Chauvelot. Increase in tumor necrosis factor-α production linked to toxicity of indomethacin in the rat small intestine. Br. J. Pharmacol. 1998; 124, 1385-94.
L Santucci, S Fiorucci, M Giansanti, PM Bounori, FM DiMatteo and A Morelli. Pentoxifylline prevents indomethacin induced acute gastric mucosal damage in rats: Role of tumor necrosis factor alpha. Gut 1994; 35, 909-15.
MB Grisham, KP Pavlick, FS Laroux, J Hoffnan, S Bharwani and RE Wolf. Nitric oxide and Chronic Gut Inflammation: Controversies in inflammatory bowel disease. J. Investig. Med. 2002; 50, 272-83.
CB Appleyard, DM, McCafferty, AW Tigley, MG Swain and JL Wallace. Tumor necrosis factor mediation of NSAID-induced gastric damage: Role of leukocyte adherence. Am. J. Physiol. 1996; 270, G42-G48.
MS Leite, P Pacheco, RN Gomes, AT Guedes, HC Castro-Faria-Neto and PT Bozza. Mechanism of increased survival after lipopolysaccharide-induced endotoxic shock in mice consuming olive oil-enriched diet. Shock 2005; 23, 173-8.
A Tanaka, H Araki, Y Komoike, S Hase and K Takeuchi. Inhibition of COX-1 and COX-2 is required for development of gastric damage in response to nonsteroidal anti-inflammatory drugs. J. Physiol. Paris. 2001; 95. 21-7.
BL Slomiany and A Slomiany. Role of ERK and p38 mitogen activated protein kinase cascades in gastric mucosal inflammatory responses to H. pylori lipopolysaccharide. Int. Union Biochem. Mol. Biol. Life 2001; 51, 315-20.
B Polat, H Suleyman and HH Alp. Adaptation of rat gastric tissue against indomethacin toxicity. Chem. Biol. Interact. 2010; 186, 82-9.
M Gennett, MT Myhre, S Abraham and LJ Egan. Metalloprotease disintegrin-mediated ectodomain shedding of EGFR ligands promotes intestinal epithelial restitution. Am. J. Physiol. Gastrointest Liver Physiol. 2004; 287, G1213-G1219.
A Tarnawski, J Stachura, T Durbin, IJ Sarfeh and H Gergely. Increased expression of epidermal growth factor receptor during gastric ulcer healing in rats. Gastroenterology 1992; 102, 695-8.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2018 Walailak Journal of Science and Technology (WJST)

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.