A Path Analysis of Psychotic Symptoms among Persons with Schizophrenia using Methamphetamines
DOI:
https://doi.org/10.48048/wjst.2019.4057Keywords:
Coping strategies, methamphetamines, path analysis, psychotic symptoms, schizophrenia, self-efficacyAbstract
Knowledge of psychotic symptoms among persons with schizophrenia influenced by methamphetamine use guides the design of nursing innovations to maximize positive patient outcomes. This cross-sectional, descriptive correlation study aimed to explore the relationships among coping, medication use self-efficacy, expressed emotions, stressful life events, social support, and social dysfunction, and to test a model that explained the influences of these factors on psychotic symptoms among persons with schizophrenia using methamphetamines.
The stress-vulnerability model for schizophrenia guided this study. A sample of 313 persons with schizophrenia using methamphetamines in psychiatric hospitals and institutes for drug abuse treatment in Thailand was recruited by multi-stage sampling and responded to a Demographic Questionnaire, Brief Psychiatric Rating Scale, Brief COPE, Self-efficacy for Appropriate Medication Use Scale, Expressed Emotional Scale, Stressful Life Events Questionnaire, and Social Dysfunction Scale. A linear structural relationship was used to test the hypothesized path model.
The hypothesized model was found to fit the empirical data and explained 54 % of variance in psychotic symptoms (χ2 = 8.28, df = 8, χ2 /df = 1.0, GFI = 0.99, AGFI = 0.96, RMSEA = 0.01). The highest total effect and factors directly affecting psychotic symptoms were emotionally focused coping strategies, medication use self-efficacy, social dysfunction, positively expressed emotions, and stressful life events.
The findings recommend that emotionally focused coping strategies, self-efficacy in medication use, social dysfunction, positively expressed emotions, and stressful life events were important factors that influenced psychotic symptoms in patients. Nursing interventions designed to manage these factors are crucial for reducing psychotic symptoms.Downloads
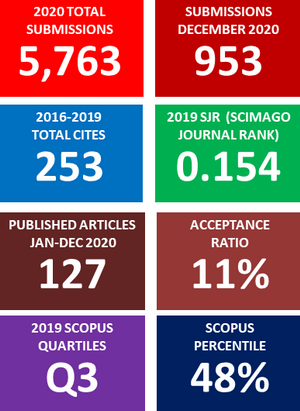
Metrics
References
J Westermeyer. Comorbid schizophrenia and substance abuse: A review of epidemiology and course. Am. J. Addict. 2006; 15, 345-55.
JY Khokhar, LL Dwiel, AM Henricks, WT Doucette and AI Green. The link between schizophrenia and substance use disorder: A unifying hypothesis. Schizophr. Res. 2018; 194, 78-85.
BJ Sadock, VA Sadock and P Ruiz. Kaplan & Sadock's Synopsis of Psychiatry: Behavioral Sciences/clinical Psychiatry. Wolters Kluwer, Philadelphia, 2015, p. 1273-8.
TL Patterson and OR Leeuwenkamp. Adjunctive psychosocial therapies for the treatment of schizophrenia. Schizophr. Res. 2008; 100, 108-19.
GW Stuart. Principles and Practice of Psychiatric Nursing. Elsevier, Missouri, 2013, p. 433-73.
KH Nuechterlein and ME Dawson. A heuristic vulnerability/stress model of schizophrenic episodes. Schizophr. Bull. 1984; 10, 300-12.
MM Kurtz, RH Olfson and J Rose. Self-efficacy and functional status in schizophrenia: Relationship to insight, cognition and negative symptoms. Schizophr. Res. 2013; 145, 69-74.
CM Hultman, IM Wieselgren and A Öhman. Relationships between social support, social coping and life events in the relapse of schizophrenic patients. Scand. J. Psychol. 1997; 38, 3-13.
NM Docherty, A St-Hilaire, JM Aakre, JP Seghers and AM Cleery and M Divilbiss. Anxiety interacts with expressed emotion criticism in the prediction of psychotic symptom exacerbation. Schizophr. Bull. 2011; 37, 611-8.
N Pujo. 2014, Schizophrenia and Stressful Life Events: Correlations with Negative and Positive Symptoms. Ph. D. Dissertation. The Chicago School of Professional Psychology, California, USA.
BG Tabachnick and LS Fidell. Using Multivariate Statistics. Pearson, Harlow, 2014, p. 666.
P Kittirattanapiboon. Brief Psychiatric Rating Scale (BPRS). Suanprung Psychiatric Hospital, 2001.
CS Carver. You want to measure coping but your protocol's too long: Consider the brief COPE. Int. J. Behav. Med. 1997; 4, 92-100.
P Rapin, A Yupin and T Sureeporn. Medication adherence among persons with post-acute myocardial infarction. Songklanakarin J. Sci. Tech. 2016; 38, 611-20.
W Nardnapa, Y Jintana and S Sunisa. Discriminant Analysis of Relapse and Non-relapse in Thai Muslim Schizophrenic Patients. Master thesis. Chulalongkorn University, Bangkok, Thailand.
H Roohafza, M Ramezani, M Sadeghi, M Shahnam, B Zolfagari and N Sarafzadegan. Development and validation of the stressful life event questionnaire. Int. J. Public Health 2011; 56, 441-8.
S Hanucharurnkul. 1988, Social Support, Self-care, and Quality of Life in Cancer Patients Receiving Radiotherapy in Thailand. Ph.D. Dissertation. Wayne State Uiversity, Michigan, USA.
N Saraswat, K Rao, DK Subbakrishna and BN Gangadhar. The Social Occupational Functioning Scale (SOFS): A brief measure of functional status in persons with schizophrenia. Schizophr. Res. 2006; 81, 301-9.
E López-Navarro, CD Canto, A Mayol, O Fernández-Alonso and E Munar. Psychotic symptoms and quality of life: A mediation analysis of daily-life coping. Psychiat. Res. 2018; 262, 505-9.
C Leclerc, AD Lesage, N Ricard, T Lecomte and M Cyr. Assessment of a new rehabilitative coping skills module for persons with schizophrenia. Am. J. Orthopsychiat. 2000; 70, 380-8.
PT Yanos. Proactive coping among persons diagnosed with severe mental illness: An exploratory study. J. Nerv. Ment. Dis. 2001; 189, 121-3.
PW Corrigan and R Toomey. Interpersonal problem solving and information processing in schizophrenia. Schizophr. Bull. 1995; 21, 395-403.
PW Lee, F Lieh-Mak, KK Yu and JA Spinks. Coping strategies of schizophrenic patients and their relationship to outcome. Br. J. Psychiat. 1993; 163, 177-82.
C Ruzibiza, R E Grattan, R Eder and RJ Linscott. Components of schizophrenia liability are not uniformly associated with stress sensitivity, resilience, and coping. Psychiat. Res. 2018; 260, 10-6.
KT Mueser, DP Valentiner and J Agresta. Coping with negative symptoms of schizophrenia: Patient and family perspectives. Schizophr. Bull. 1997; 23, 329-39.
MK Sharma and P Mahindru. Online methods of managing auditory hallucinations: A new trend to understand psychopathology. Indian J. Psychol. Med. 2017; 39, 354-6.
PH Lysaker, GJ Bryson, RS Lancaster, JD Evans and MD Bell. Insight in schizophrenia: associations with executive function and coping style. Schizophr. Res. 2003; 59, 41-7.
KE Wilder-Willis, PK Shear, JJ Steffen and J Borkin. The relationship between cognitive dysfunction and coping abilities in schizophrenia. Schizophr. Res. 2002; 55, 259-67.
G Singh, P Sharan and P Kulhara. Role of coping strategies and attitudes in mediating distress due to hallucinations in schizophrenia. Psychiat. Clin. Neurosci. 2003; 57, 517.
CJ Asher and L Gask. Reasons for illicit drug use in people with schizophrenia: Qualitative study. BMC Psychiat. 2010; 10, 94-108.
L Wang, SK Lin, YC Chen, MC Huang, TT Chen, SC Ree and CK Chen. Differences in clinical features of methamphetamine users with persistent psychosis and patients with schizophrenia. Psychopathology 2016; 49, 108-15.
M Lammertink, F Löhrer, R Kaiser, M Hambrecht and R Pukrop. Differences in substance abuse patterns: multiple drug abuse alone versus schizophrenia with multiple drug abuse. Acta Psychiat. Scand. 2001; 104, 361-6.
FW O'Connor. A vulnerability-stress framework for evaluating clinical interventions in schizophrenia. Image J. Nurs. Scholar. 1994; 26, 231-7.
T Domínguez-Martínez, C Medina-Pradas, TR Kwapil and N Barrantes-Vidal. Relatives' expressed emotion, distress and attributions in clinical high-risk and recent onset of psychosis. Psychiat. Res. 2017; 247, 323-9.
E Villard, C Vedie, C Lenoir and M Faure. Schizophrenic relapses: Correlation between life events and rehospitalization. Ann. Méd. Psychol. 2015; 173, 443-8.
JY Guo, S Huhtaniska, J Miettunen, E Jääskeläinen, V Kiviniemi, J Nikkinen, J Moilanen, M Haapea, P Mäki, PB Jones, V J eijola, M Isohanni and GK Murray. Longitudinal regional brain volume loss in schizophrenia: Relationship to antipsychotic medication and change in social function. Schizophr. Res. 2015; 168, 297-304.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2018 Walailak Journal of Science and Technology (WJST)

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.