Factors Influencing Adherence to Preventive Behaviors among Thais with Hypertension: A Literature Review
DOI:
https://doi.org/10.48048/wjst.2019.3863Keywords:
Adherence, preventive behaviors, hypertension, Thai patients, reviewAbstract
The purpose of this study was to summarize empirical evidence regarding factors influencing adherence to preventive behaviors of Thais with hypertension. An electronic search was performed using PubMed, Medline, CINAHL, SCOPUS, ThaiJo, and ThaiLis databases to identify studies that examined the factors which influenced adherence to preventive behaviors in Thai adults with hypertension. We identified research studies published between 1995 and 2017, which were assessed by 2 independent reviewers. Fourteen publications were included; 3 of these were qualitative studies. Social support, knowledge of hypertension, perception of illness, perceived benefits, perceived barrier, perceived self-efficacy, Thai cultural values, and patient-provider communication were identified as factors influencing adherence to preventive behaviors of Thai adults with hypertension. Although information about factors influencing adherence is growing, more research is needed on how to provide the best intervention support for this challenging task.Downloads
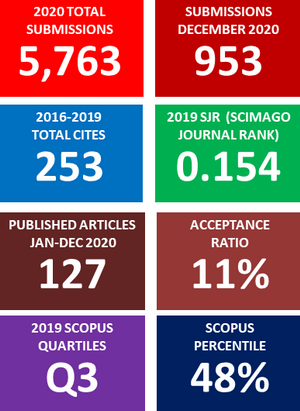
Metrics
References
P Muntner, BR Davis, WC Cushman, S Bangalore, DA Calhoun, SL Pressel, HR black, JB Kostis, JL Probstfield, PK Whelton and M Rahman. Treatment-resistant hypertension and the incidence of cardiovascular disease and end-stage renal disease: Results from the antihypertensive and lipidlowering treatment to prevent heart attack trial (ALLHAT). Hypertension 2014; 64, 1012-21.
Y Wang, J Xu, X Zhao, D Wang, C Wang, L Liu, A Wang, X Meng, H Li and Y Wang. Association of hypertension with stroke recurrence depends on ischaemic stroke subtype. Stroke 2013; 44, 1232-7.
NCD Risk Factor Collaboration. Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population based measurement studies with 19.1 million participants. Lancet 2017, 389, 37-55.
W Aekplakorn, R Sangthong, P Kessomboon, P Putwatana, R Inthawong, S Taneepanichskul, P Piyamitr, S Sangwatanaroj and S Chariyalertsak. Changes in prevalence, awareness, treatment and control of hypertension in Thai population, 2004-2009: Thai National Health Examination Survey III-IV. J. Hypertens. 2012; 30, 1734-42.
W Aekplakorn. Thailand National Health Examination Survey V. Health System Research Institute, Nonthaburi, Thailand, 2016.
AV Chobanian, GL Bakris, HR Black, WC Cushman, LA Green, JL Izzo, DW Jones, BJ Materson, S Oparil, JT Wright, JR Toccella and EJ Rocella. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003; 42, 1206-52.
S Vooradi and UV Mateti. A systemic review on lifestyle interventions to reduce blood pressure. J. Health Res. Rev. 2016; 3, 1-5.
HO Dickinson, JM Mason, DJ Nicolson, F Campbell, FR Beyer, JV Cook, B Williams and GA Ford. Lifestyle interventions to reduce raised blood pressure: A systematic review of randomized controlled trials. J. Hypertens. 2006; 24, 215 33.
E Sabate. Adherence to Long-Term Therapies: Evidence for Action. Geneva, Switzerland, World Health Organization, 2003.
S Chongthawonsatid. Demographic factors and health care behavior of hypertension disease in Thailand (in Thai). Silpakorn Univ. Sci. Tech. J. 2015; 9, 9-16.
A Tibebu, D Mengistu and L Negesa. Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Patient Prefer. Adher. 2017; 11, 323-30.
Joanna Briggs Institute. Available at: http://joannabriggs.org/assets/docs/sumari/Reviewers-Manual_Methodology-for-JBI-Scoping-eviews_2015_v2.pdf, accessed February 2017.
P Chonsin, C Kaveevivitchai, N Neelapaichit and N Piaseu. Impact of a blood pressure regulating programme on health beliefs, health behaviour, amount of sodium intake and hypertension levels in community members with hypertension (in Thai). Thai J. Nurs. Council 2016; 31, 63-75.
L Saleema, O Panpakdee, M Arpanantikul and T Chai-Aroon. The influence of basic conditioning factors and self-care agency on self-care behaviors in Thais with hypertension. Pac. Rim. Int. J. Nurs. Res. 2016; 20, 5-17.
P Sangprasert, S Buranatrevedh and D Pipatsatitpong. The effectiveness of hypertensive management programs and social support in primary health care systems: Preliminary study. Siriraj Med. J. 2016; 68, 369-76.
S Leelacharas, J Chontichachalalauk and W Snongdech. Dietary-taking, exercise, and medication adherence in Thais with hypertension based on gender, age, and educational level (in Thai). J. Public Health Nurs. 2015; 29, 56-70.
N Piaseu, N Thaothong, S Jarupat Maruo and S Piyatrakul. Effects of community participation program for blood pressure control on health behaviors and blood pressure in community dwellers with hypertension. J. Hypertens. 2015; 33, e149.
S Jianvitayakij, O Panpakdee and P Malathum, S Duffy and C Viwatwongkasem. Factors influencing smoking cessation behavior among Thai male smokers with hypertension. Pac. Rim. Int. J. Nurs. Res. 2014; 18, 100-10.
E Pinprapapan, S Panuthai, T Vannarit and W Srisuphan. Casual model of adherence to therapeutic regimens among Thais with hypertension. Thai J. Nurs. Res. 2013; 17, 268-81.
P Srison, K Masingboon and S Duangpaeng. Relationship between client-professional interaction and adherence to treatment among persons with hypertension (in Thai). J. Facul. Nurs. Burapha Univ. 2011; 17, 60-74.
T Houmkhuntod and S Preechawong. Effects of perceived self-efficacy promoting program on dietary consumption and exercise behaviors among hypertensive patients (in Thai). J. Nurs. Sci. Health 2009; 32, 19-28.
S Limcharoen, K Masingboon and W Kunsongkeit. Factors related to adherence to treatment among essential hypertensive patients (in Thai). J. Facul. Nurs. Burapha Univ. 2007; 15, 63-79.
S Tantayothin. 2004, Factors Influencing Nutritional and Exercise Behaviors of Hypertension Patients in Sainoi District. Master Degree, Dissertation. Mahidol University, Bankok, Thailand.
VA Braithwaite and WA Scott. “Values,” in Measures of Personality and Social Psychological Attitudes. In: JP Robinson, PR Shaver and LS Wrightsman (Eds.). Academic Press, Burlington, 1991, p. 661-776.
S Naewbood, S Sorajjakool and SK Triamchaisri. The role of religion in relation to blood pressure control among a Southern California Thai population with hypertension. J. Relig. Health 2012; 51, 187-97.
S Huangtong, N Piaseu and C Kaveevivitchai. Case study: Behaviors, problems, and barriers of blood pressure control in persons with severe hypertension in a Community. Ramathibodi Nurs. J. 2013; 19, 129-42.
W Kirdphon. 2003, Accepting and Adjusting to Chronicity of Hypertension: A Grounded Theory Study in Thai People. Ph.D. Dissertation, University of Washington, United States.
ME Magrin, M D Addario, A Greco, M Miglioretti, M Sarini, M Scrignaro, P Steca, L Vecchio and E Crocetti. Social support and adherence to treatment in hypertensive patients: A meta-analysis. Ann. Behav. Med. 2015; 49, 307-18.
OS Ojo, SO Malomo, PT Sogunle and AM Ige. Blood pressure (BP) control and perceived family support in patients with essential hypertension seen at a primary care clinic in Western Nigeria. J. Fam. Med. Prim. Care 2016; 5, 569-75.
M Kilic, T Uzunçakmak and H Ede. The effect of knowledge about hypertension on the control of high blood pressure. Int. J. Cardiovasc. Acad. 2016; 2, 27-32.
ARA Rahman, JG Wang, GMY Kwong, DD Morales, P Sritara and R Sukmawan. Perception of hypertension management by patients and doctors in Asia: Potential to improve blood pressure control. Asia Pac. Fam. Med. 2015; 14, 2.
MR DiMatteo, KB Haskard and SL Williams. Health beliefs, disease severity, and patient adherence: A meta-analysis. Med. Care 2007; 45, 521-8.
K Park, S Cho and JK Bower. Changes in adherence to non-pharmacological guidelines for hypertension. PLoS One 2016; 11, e0161712.
SO Ike, PN Aniebue and UU Aniebue. Knowledge and perceptions related to hypertension, lifestyle behavior modifications and challenges that facing hypertensive patients. IOSR J. Nurs. Health Sci. 2015; 4, 15-26.
CJ Carpenter. A meta-analysis of the effectiveness of the health belief model variables in predicting behavior. Health Comm. 2010; 25, 661-9.
A Bandura. Self-Efficacy: The Exercise of Control. Freeman, New York, 1997, p. 36-38.
J Warren-Findlow, RB Seymour and LR Brunner Huber. The association between self-efficacy and hypertension self-care activities among African American adults. J. Comm. Health 2012; 37, 15-24.
LL Lee, A Arthur and M Avis. Using self-efficacy theory to develop interventions that help older people overcome psychological barriers to physical activity: A discussion paper. Int. J. Nurs. Stud. 2008; 45, 1690-9.
S Byrne, D Barry and NM Petry. Predictors of weight loss success: Exercise vs dietary self-efficacy and treatment attendance. Appetite 2012; 58, 695-8.
E Martinez, KL Tatum, M Glass, A Bernath, D Ferris, P Reynolds and R Schnoll. Correlates of smoking cessation self-efficacy in a community sample of smokers. Addict. Behav. 2010; 35, 175-8.
O Panpakdee, W Sritanyarat and S Tanomsup. Self-care process in Thai people with hypertension: An emerging model. Thai. J. Nurs. Rese. 2003; 7, 121-36.
S Naewbood, S Sorajjakool and SK Triamchaisri. The role of religion in relation to blood pressure control among a Southern California Thai population with hypertension. J. Relig. Health 2012; 51, 187-97.
B Naemiratch and L Manderson. Control and adherence: Living with diabetes in Bangkok, Thailand. Soc. Sci. Med. 2006; 63, 1147-57.
S Chukumnird, U Boonyasopun and P Jittanoon. Perspectives regarding adherence to preventive behaviors: A qualitative study of Thais with prehypertension. Pac. Rim. Int. J. Nurs. Res. 2016; 20, 106-18.
KB Zolnierek and MR DiMatteo. Physician communication and patient adherence to treatment: A meta-analysis. Med. Care 2009; 47, 826-34.
C Stavropoulou. Non-adherence to medication and doctor-patient relationship: Evidence from a European survey. Patient Educ. Couns. 2011; 83, 7-13.
M Baumann, A Tchicaya, N Lorentz and EL Bihan. Impact of patients’ communication with the medical practitioners, on their adherence declared to preventive behaviours, five years after a coronary angiography, in Luxembourg. PLoS One 2016; 11, e0157321.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2018 Walailak Journal of Science and Technology (WJST)

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.