TB Treatment with DOT: RCT vs. Effective Program Management
Keywords:
Tuberculosis, DOT, RCTAbstract
In the area of Directly-Observed Treatment (DOT), one of 5 essential elements of Directly-Observed Treatment, Short-course (DOTS)- the internationally accepted strategy to combat tuberculosis (TB) promoted by the World Health Organization (WHO) - its usefulness has been continuously debated. Many researchers have tried to conduct randomized controlled trials (RCT) to explore its effectiveness. The results have always led to the conclusion that DOT and self-administration (SA) could produce the same treatment outcomes. However, RCT should be conducted under ideal conditions to develop the efficacy of TB drug regimens, and it may not be necessary for it to be conducted in the field under routine circumstances to find out the effectiveness. Instead of RCT, effective management is needed in the fields, both at program level and at individual level, to produce TB treatment outcomes that come close to the efficacy of TB drug regimens.
doi:10.14456/WJST.2015.70
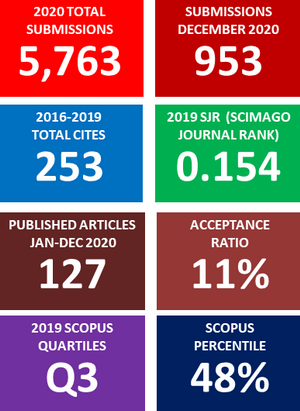
Downloads
Metrics
References
World Health Organization. TB: A Global Emergency. WHO/TB/94.177, WHO, Geneva, Switzerland, 1994.
World Health Organization. Global Tuberculosis Report 2014. WHO/HTM/TB/2014.08, France, 2014.
World Health Organization. Treatment of Tuberculosis: Guidelines for National Programmes. 3rd ed. WHO/CDS/TB/2003.313, Italy, 2003.
JM Last. A Dictionary of Epidemiology. 4th ed. Oxford University Press, New York, 2001.
AL Cochrane. Effectiveness and Efficiency; Random Reflections on Health Services. Nuffield Provincial Hospitals Trust, London, 1972.
World Health Organization. Toman’s Tuberculosis Case Detection, Treatment, and Monitoring: Questions and Answers. 2nd ed. WHO/HTM/TB/2004.334, China, 2004.
A Jindani, AJ Nunn and DA Enarson. Two 8-month regimens of chemotherapy for treatment of newly diagnosed pulmonary tuberculosis: International multicentre randomised trial. Lancet 2004; 364, 1244-51.
ID Rusen, N Aït-Khaled, E Alarcón, N Billo, K Bissell, F Boillot, J Caminero, CY Chiang, P Clevenbergh, P Dhliwayo, R Dlodlo, DA Enarson, O Ferroussier, PI Fujiwara, E Heldal, SG Hinderaker, SJ Kim, C Lienhardt, HL Rieder, A Trébucq, AV Deun and N Wilson. Cochrane systematic review of directly observed therapy for treating tuberculosis: Good analysis of the wrong outcome. Int. J. Tuberc. Lung Dis. 2007; 11, 120-1.
M Zwarenstein, JH Schoeman, C Vundule, CJ Lombard and M Tatley. Randomised controlled trial of self-supervised and directly observed treatment of tuberculosis. Lancet 1998; 352, 1340-3.
P Kamolratanakul, H Sawert, S Lertmaharit, Y Kasetjaroen, S Akksilp, C Tulaporn, K Punnachest, S Na-Songkhla and V Payanandana. Randomized controlled trial of directly observed treatment (DOT) for patients with pulmonary tuberculosis in Thailand. Tran. R. Soc. Trop. Med. Hyg. 1999; 93, 552-7.
M Zwarenstein, JH Schoeman, C Vundule, CJ Lombard and M Tatley. A randomised controlled trial of lay health workers as direct observers for treatment of tuberculosis. Int. J. Tuberc. Lung Dis. 2000; 4, 550-4.
JD Walley, MA Khan, JN Newell and MH Khan. Effectiveness of the direct observation component of DOTS for tuberculosis: A randomised controlled trial in Pakistan. Lancet 2001; 357, 664-9.
F Lwilla, D Schellenberg, H Masanja, C Acosta, C Galindo, J Aponte, S Egwaga, B Njako, C Ascaso, M Tanner and P Alonso. Evaluation of efficacy of community-based vs. institutional-based direct observed short-course treatment for the control of tuberculosis in Kilombero district, Tanzania. Trop. Med. Int. Health 2003; 8, 204-10.
CR Maclntyre, K Goebel, GV Brown, S Skull, M Starr and RO Fullinfaw. A randomised controlled clinical trial of the efficacy of family-based direct observation of anti-tuberculosis treatment in an urban, developed-country setting. Int. J. Tuberc. Lung Dis. 2003; 7, 848-54.
J Wright, J Walley, A Philip, S Pushpananthan, E Dlamini, J Newell and S Dlamini. Direct observation of treatment for tuberculosis: A randomized controlled trial of community health workers versus family members. Trop. Med. Int. Health 2004; 9, 559-65.
E Wandwalo, N Kapalata, S Egwaga and O Morkve. Effectiveness of community-based directly observed treatment for tuberculosis in an urban setting in Tanzania: A randomised controlled trial. Int. J. Tuberc. Lung Dis. 2004; 8, 1248-54.
JN Newell, SC Baral, SB Pande, DS Bam and P Malla. Family-member DOTS and community DOTS for tuberculosis control in Nepal: Cluster-randomised controlled trial. Lancet 2006; 367, 903-9.
J Volmink and P Garner. Directly observed therapy for treating tuberculosis (Review). The Cochrane Collaboration, 2009, Issue 1, Available at: www.thecochranelibrary.com/userfiles/ccoch/ file/CD003343.pdf, accessed October 2014.
Centers for Disease Control and Prevention, United States of America. Improving Patient Adherence to Tuberculosis Treatment, Revised 1994. Centers for Disease Control and Prevention, Atlanta, USA, 1994.
World Health Organization. Tuberculosis Handbook. WHO/TB/98.253, Italy, 1998.
P Rattanasuwan, C Yuanlae and P Daewa. DOT (Directly-Observed Treatment) by assigning other persons who were not family members: A model of 11th Zonal Tuberculosis Center, Nakhon Si Thammarat in the fiscal year 1999-2000 (in Thai). Songkla. Med. J. 2002; 20, 69-78.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.